Toxic Cough Syrup Tragedy: Centre Orders States to Review Pediatric Medicines
By: Javid Amin | 05 October 2025
National Health Emergency: Toxic Cough Syrup Claims 11 Young Lives
India is reeling from yet another pharmaceutical tragedy. The Union Health Ministry has ordered all states and Union Territories to review and regulate the use of cough syrups, following the deaths of 11 children in Madhya Pradesh’s Ujjain district.
Preliminary investigations confirmed the cause: a toxic batch of pediatric cough syrup contaminated with diethylene glycol (DEG) — a deadly industrial solvent known to cause acute kidney failure.
The syrup, manufactured by a Tamil Nadu–based pharmaceutical company, was widely distributed through local clinics and unverified pharmacies, exposing serious gaps in India’s drug safety chain.
The Tragedy Unfolds: Deaths, Arrests, and Accountability
The case came to light after several children in Ujjain and nearby districts reported vomiting, confusion, and renal distress. Within days, 11 young patients succumbed, sparking a state-wide alert.
Authorities have since:
-
Arrested a local doctor accused of prescribing the syrup without verifying its source.
-
Booked the manufacturing company under the Drugs and Cosmetics Act and IPC Sections for Culpable Homicide.
-
Ordered the Central Drugs Standard Control Organisation (CDSCO) to seal the factory and conduct a nationwide audit of similar syrup formulations.
“This is a national emergency in slow motion. One negligent batch can undo years of public health progress,” said a senior CDSCO official.
What Went Wrong: A Forensic Breakdown
The forensic and toxicology reports revealed chilling details:
-
The syrup contained dangerously high levels of diethylene glycol (DEG)—a solvent meant for industrial use, not human consumption.
-
No quality control certification was issued for the batch.
-
Misleading labels omitted safety warnings and batch details.
-
The syrup bypassed regulatory checks, entering pharmacies through unauthorized distribution channels.
Diethylene glycol has been responsible for multiple mass poisonings worldwide—from Panama (2006) to Gambia (2022)—and now, once again, in India.
“The tragedy in Ujjain echoes a pattern we’ve seen too many times—cheap shortcuts, poor oversight, and avoidable deaths,” said Dr. A.K. Singh, former director of the National Institute of Biologicals.
Centre’s Directive: Rational Use and Stringent Oversight
The Union Health Ministry, in an advisory issued to all states and UTs, has called for immediate and systemic action to prevent another such disaster.
Key Measures Ordered:
-
🔍 Comprehensive audit of all pediatric cough syrup stocks.
-
⚗️ Batch-wise testing of formulations before public distribution.
-
📦 Stricter enforcement of labeling, licensing, and manufacturing norms.
-
📢 Public awareness drives on safe medication and counterfeit detection.
-
🧾 Mandatory reporting of adverse drug reactions through national portals.
State drug inspectors, pediatric associations, and pharmacists have been instructed to coordinate in real time for early detection of contaminated products.
“We are dealing with a systemic failure, not an isolated error. Rational prescribing and stronger pharmacovigilance are non-negotiable,” said a Health Ministry spokesperson.
Public Health Experts React: ‘This Was Preventable’
Across India, medical professionals and health policy experts have condemned the tragedy as a failure of regulation and ethics.
Dr. Rukhsana Mir, a pediatrician based in Srinagar, said:
“This tragedy was preventable. We need systemic reform, not reactive bans. Children are not test subjects for poorly regulated drugs.”
Health advocates are demanding:
-
A national registry for pediatric drug formulations.
-
Real-time pharmacovigilance to track side effects.
-
Toxicology education as part of medical training.
-
Harsher penalties for negligent manufacturers and distributors.
Why Kashmir and Other UTs Must Be Extra Vigilant
The directive carries special importance for Jammu & Kashmir, where healthcare infrastructure remains uneven and rural access to pediatric specialists is limited.
Local authorities have launched audits of rural clinics and chemist shops, particularly focusing on imported and unverified syrup brands sold without prescription.
Tourism operators, including JKL Travels, have also issued advisories for visiting families:
“Parents traveling with children should carry doctor-prescribed medicines and avoid buying unbranded syrups locally,” said the company’s spokesperson.
In regions where medical oversight is fragmented, the Centre’s directive may prove lifesaving.
Legal and Policy Fallout: Toward Safer Medicines
The Ujjain case is expected to reshape drug policy enforcement. The Tamil Nadu manufacturer faces charges of culpable homicide, with the CDSCO now retesting 120 batches of similar syrups across the country.
Legal experts note that under the Drugs and Cosmetics Act (1940), producing adulterated or spurious medicines is punishable by imprisonment up to life.
However, weak enforcement and political lobbying have long diluted accountability. Activists are now urging Parliament to pass amendments mandating criminal liability for corporate negligence in pharmaceutical safety.
The Science of Poison: Understanding Diethylene Glycol
Diethylene Glycol (DEG) is a clear, sweet-tasting chemical commonly used in antifreeze, paints, and industrial solvents.
When ingested, even in small doses, it can destroy kidney and liver cells, leading to acute renal failure, neurological damage, and death.
Toxicologists warn that DEG contamination often occurs when manufacturers replace expensive pharmaceutical-grade solvents with industrial substitutes to cut costs.
“It’s an invisible killer. The syrup may look fine, but inside it’s a chemical trap,” said Dr. Feroz Ahmad, toxicology expert at SKIMS Srinagar.
Lessons from the Past: India’s Recurring Pharmaceutical Scandals
India’s pharmaceutical industry, while a global exporter, has seen repeated safety lapses:
-
1998 – Delhi: 33 children died after consuming contaminated paracetamol syrup.
-
2019 – Jammu: Fake antibiotics seized from an unlicensed factory.
-
2022 – Gambia: 66 children died after taking syrup made by an Indian company.
Despite reforms, weak inspections and counterfeit circulation continue to plague the supply chain. Experts say the Ujjain incident is a warning bell to overhaul quality assurance mechanisms.
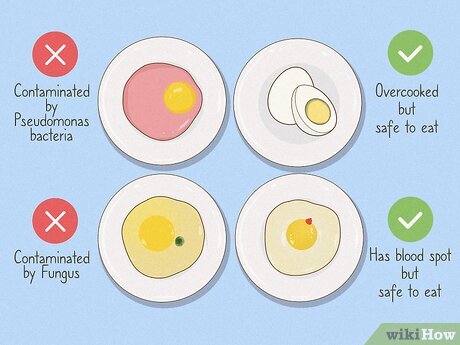
What Parents and Consumers Should Know
The Health Ministry has urged parents to stay alert when purchasing medicines for children.
Safety Checklist for Cough Syrups:
-
✅ Buy only from licensed pharmacies.
-
✅ Check manufacturer’s name, batch number, and expiry date.
-
⚠️ Avoid unsealed or repackaged bottles.
-
🔎 Verify FSSAI or CDSCO approval on the label.
-
🚫 Do not rely on self-medication or local substitutes.
Parents are also encouraged to report suspicious or adverse drug reactions via the Central Drug Monitoring (CDM) portal.
The Road Ahead: Restoring Trust in India’s Medicines
The tragedy in Ujjain has reignited a national debate on drug manufacturing ethics, pediatric safety, and regulatory transparency.
Experts agree that public trust in Indian pharmaceuticals—domestically and globally—depends on the government’s ability to ensure accountability, traceability, and quality control.
“The loss of 11 children is not just a local issue; it’s a wake-up call for an entire system,” said Dr. Meera Bhattacharya, public health policy analyst.
“Every child deserves medicine that heals, not harms.”
Bottom-Line
The Ujjain cough syrup tragedy stands as a grim reminder that safety shortcuts in medicine can cost the most innocent lives.
As India moves to tighten controls, the challenge lies in implementation—not intention.
Every bottle, every prescription, and every pharmacy must now reflect a single truth:
In matters of child health, there is no margin for error.